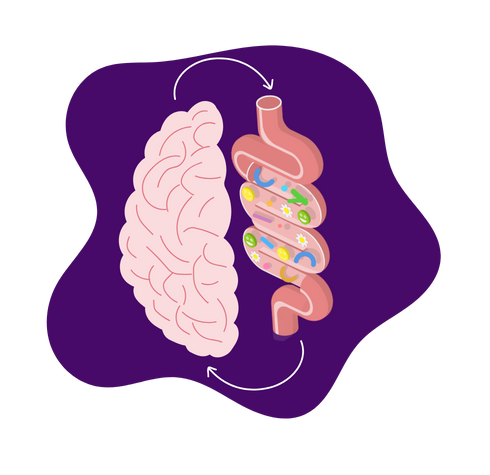
The human gut microbiome is an intricate community of trillions of bacteria, viruses, and fungi. After decades of research, scientists now understand that the gut and brain engage in constant, sophisticated communication through multiple biological pathways known as the gut-brain axis. This bidirectional signaling system means that the state of our gut microbiome doesn’t just affect digestion but also influences mood, cognition, and even our risk for neurological disorders.
Recent research has revealed connections between gut microbial imbalances and conditions like depression, anxiety, Alzheimer’s disease, and Parkinson’s disease. The mechanisms behind these links involve interactions among the nervous system, immune function, and microbial metabolites. As we continue to unravel these relationships, it’s becoming clear that exploring gut health may be one of the most promising frontiers in neuroscience and mental health.
The Science Behind Gut-Brain Communication
The gut and brain maintain their dialogue through several key pathways. The vagus nerve serves as a direct neural superhighway, transmitting signals between the digestive system and the brain. This cranial nerve carries information about our gut, which influences emotions and stress responses, while also relaying brain signals that affect digestion. Studies have demonstrated that severing the vagus nerve in animal models blocks many of the microbiome’s effects on behavior, proving its critical role in gut-brain communication.
Beyond neural connections, gut microbes produce numerous neuroactive compounds that influence brain function. A great deal of serotonin is produced in the gut by specialized cells that closely interact with gut bacteria. Serotonin plays a major role in regulating mood, sleep, and appetite. Other microbes generate gamma-aminobutyric acid, which has calming effects on the nervous system, while some produce dopamine, which affects motivation and reward processing.
The gut microbiome also shapes brain health through its production of short-chain fatty acids, which are byproducts of fiber fermentation. These molecules—particularly butyrate, propionate, and acetate—have been shown to reduce neuroinflammation, strengthen the blood-brain barrier, and even promote the growth of new neurons. Short-chain fatty acids are important because they help protect the brain from harmful inflammation and support the development and maintenance of healthy brain cells. Research indicates that people with neurodegenerative diseases often have lower levels of these beneficial short-chain fatty acids, suggesting they may help guard against brain deterioration.
Gut Microbes and Neurological Disorders
The influence of gut bacteria extends to several major neurological conditions. In depression and anxiety disorders, researchers have consistently observed gut microbiome compositions that vary from those of healthy individuals. These changes often involve reduced microbial diversity and lower levels of beneficial bacteria known to produce anti-inflammatory compounds. Interestingly, when scientists transfer gut bacteria from depressed humans to germ-free mice, the animals begin showing depressive-like behaviors, providing strong evidence for a causal relationship.
Alzheimer’s disease research has uncovered important connections to gut health as well. Certain gut bacteria appear to influence the accumulation of amyloid-beta plaques, a hallmark of Alzheimer’s pathology. This influence may be due to how microbes impact inflammation and release chemical signals that can help or harm neurons. Similarly, in Parkinson’s disease, growing evidence supports the gut-first hypothesis, where abnormal protein folding may begin in the gut before spreading to the brain. Many Parkinson’s patients experience digestive symptoms years before motor problems appear, and their gut microbiomes often differ greatly from the microbiomes of healthy individuals.
Autism spectrum disorder represents another area where gut-brain interactions are actively being studied. Many children with autism experience gastrointestinal issues, and their gut microbiomes frequently differ from those of neurotypical children. Some researchers hypothesize that certain gut bacteria may produce neuroactive compounds that influence brain development and behavior. Early clinical trials exploring microbiome-based interventions for autism have shown promising results in improving both digestive and behavioral symptoms.
Supporting Brain Health Through Gut Care
Given the growing evidence linking gut and brain health, several practical strategies may help optimize this crucial connection. Dietary approaches are among the most well-studied interventions. Consuming a diverse array of fiber-rich plants such as lentils, oats, leafy greens, and bananas nourishes beneficial gut bacteria that produce brain-healthy short-chain fatty acids. Fermented foods like yogurt, kefir, and kimchi introduce live microbes that may help maintain a balanced gut ecosystem. Polyphenol-rich foods such as berries, dark chocolate, and green tea provide additional benefits through their antioxidant properties, reducing inflammation throughout the body, including in the brain.
Lifestyle factors beyond diet also play significant roles. Regular physical exercise has been shown to increase microbial diversity and promote the growth of beneficial bacteria like Akkermansia, which helps maintain gut barrier integrity. The gut barrier is a protective lining that prevents harmful substances in the digestive tract from entering the bloodstream. Quality sleep appears to be equally important, as sleep disturbances can rapidly alter gut microbiome composition in ways that may negatively impact brain function. Stress management techniques are particularly crucial given that chronic stress can damage the gut lining, alter microbial populations, and increase inflammation—all of which may ultimately affect mental health.
Emerging therapies are taking these concepts even further. Fecal microbiota transplantation, while still experimental for neurological conditions, has shown promise in early studies for Parkinson’s disease and depression. Researchers are also developing targeted psychobiotics, which are specific probiotic strains selected for their mental health benefits. As our understanding grows, we may see more personalized approaches to microbiome-based brain health interventions.
Conclusion
The revolutionary understanding of the gut-brain axis has transformed how we think about neurological health. No longer can we consider brain function in isolation from the rest of the body—particularly the gut microbiome, which exerts profound influence through multiple interconnected pathways. While much remains to be discovered, current evidence strongly suggests that caring for our gut microbes through diet, lifestyle, and potentially targeted therapies may be one of our most powerful tools for maintaining cognitive function and emotional well-being throughout life.
Key Sources:
- Growth hormone in liver fibrosis
- Amyloid-β peptide protects against microbial infection in mouse and worm models of Alzheimer’s disease
- Gut Microbiota in Bipolar Depression and Its Relationship to Brain Function: An Advanced Exploration
- Gut Microbiota Regulate Motor Deficits and Neuroinflammation in a Model of Parkinson’s Disease
- Long-term benefit of Microbiota Transfer Therapy on autism symptoms and gut microbiota | Scientific Reports
