Clinical neuropsychology is a specialty within clinical psychology, focused on the relationships among the brain, central nervous system, cognition, and behavior. It particularly centers on brain disorders and traumatic brain injuries that may result in memory or thinking deficits. Clinical neuropsychologists commonly treat neurodevelopmental disorders (e.g., autism spectrum disorder and learning disabilities), strokes, epilepsy, brain cancer, concussions, neurological diseases, movement conditions (e.g., Parkinson’s disease), attentional disorders (e.g., ADHD), multiple sclerosis, and dementia. These conditions may be comorbid with other neuropsychiatric mental health disorders, such as depression and anxiety, especially if the patient has a family history of them. Therefore, it is important for clinical neuropsychologists to document comorbidities, as brain injury symptoms may not immediately present themselves. Consequently, if not properly informed, the clinician may overlook the anatomical and physiological ethologies.
When receiving a new patient, clinical neuropsychologists usually administer cognitive neurological assessments to test brain function. These examinations can test for a variety of cognitive functions, such as problem-solving, language, attention, memory, executive functioning, and personality. After the test results are analyzed, the clinical neuropsychologist can then diagnose their patient and proceed with treatment. The treatment is generally performed holistically and collaboratively with an interdisciplinary healthcare team, including disciplines such as neurologists, speech language pathologists, psychiatrists, neurosurgeons, and therapists, who work together to help their patient.
Once the team is established, clinical neuropsychologists work with the patient to create a tailored, comprehensive treatment plan that may include psychotherapy, cognitive rehabilitation, medication management, and modifiable lifestyle alterations. These services are beneficial to those diagnosed with neurodegenerative conditions and memory impairments, as they may support them with their attention building and recall training exercises. Such memory-stimulating activities are especially helpful, as most patients diagnosed with cognitive decline exhibit elevated levels of distress and discomfort that lowers their quality of life and negatively impacts their emotional and psychological symptoms if left untreated. For that reason, clinical neuropsychologists step in to help their patients manage their symptoms, such as by making dietary changes. Examples include educating their patients on the positive correlational data between memory and the consumption of foods containing high Omega-3 content, such as fish. Researchers speculate Omega-3 influences dementia symptoms by way of neurogenesis in the hippocampus, which is the brain’s spatial memory center. Although this is not a causal relationship, it does suggest how changes in our food intake can influence cognitive decline symptoms.
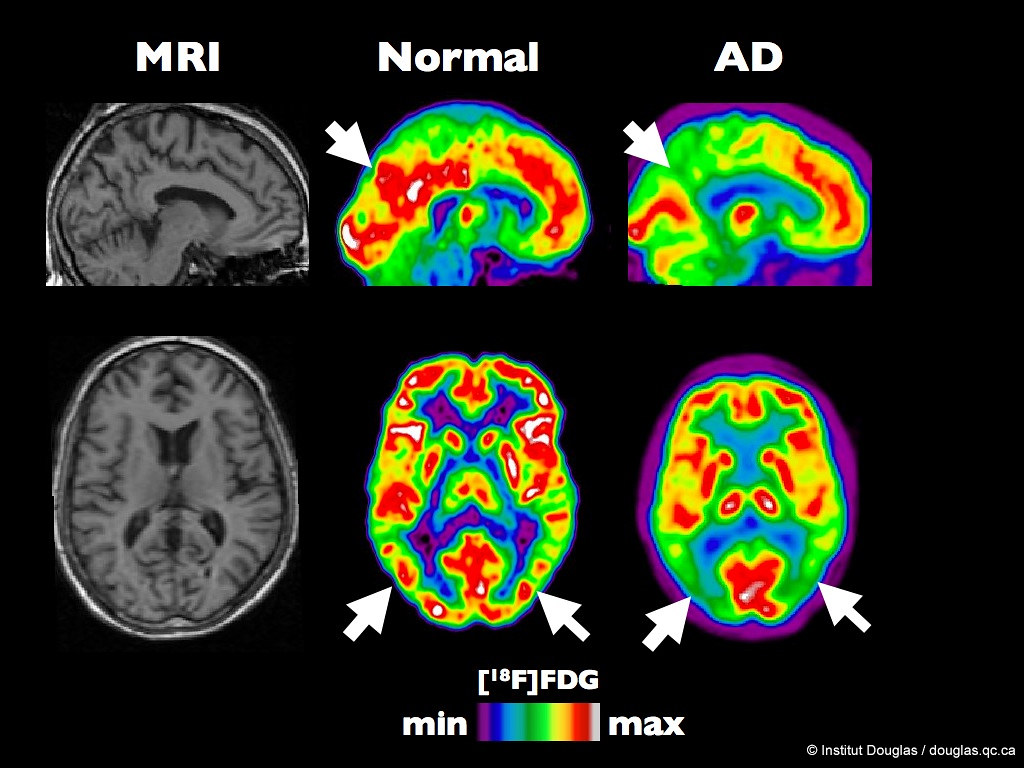
Furthermore, clinical neuropsychologists can assist with the early detection of neurodegenerative conditions through their neuropsychological assessments. For instance, if they find their patient is exhibiting mild cognitive impairment, which may be a precursor for further cognitive decline conditions, such as dementia, they would contact the appropriate medical personnel for further evaluation and prevent further progression. This may include referring the patient to a neurologist to get neuroimaging work done on their brain to further analyze these structures for damage that may explain their symptoms. The clinical neuropsychologist may also refer them to other clinicians, such as social workers and therapists for extra support. Additionally, clinical neuropsychologists can use this experience as an opportunity to educate their patients about their condition and the risks of not properly taking care of their disorder. Such information can allow their patients to make more informed decisions about their brain health before it progresses any further and affects their ability to function independently.
To test for mental health conditions, one notable neuropsychological assessment practitioners use is the Consortium to Establish a Registry for Alzheimer’s Disease Word Learning (CERAD-WL) subtest. Clinical neuropsychologists utilize the CERAD-WL when they are treating a patient they believe is at risk for neurodegenerative conditions, such as dementia or Alzheimer’s disease (AD), which are both connected with cognitive decline and memory loss. The CERAD-WL assessment is first performed by the examiner by verbally presenting a list of words to participants. After that, participants are asked to immediately recall the list that was presented to them just moments prior. Then, the clinical neuropsychologist distracts participants for a brief moment to create a delay. Once enough time has elapsed, participants are asked to recall the list of items again. How participants respond to this latter memory performance task is what clinicians use to distinguish and diagnose those who have dementia or AD versus those who do not. They do this by comparing the participant’s scores relative to the standardized normative sample values from those who hold similar demographic identities or statuses to the patients.
As the treatment plan progresses, clinical neuropsychologists keep track of their patients’ cognitive changes by routinely performing these psychological assessments. Such forms of analysis can help them and the healthcare team determine which part of the brain is negatively impacted. Following their patients’ performance will dictate the next course of action within the treatment plan and where clinicians should direct their attention to. This is important for practitioners to do as where, when, and how they administer their services could mean the difference between life and death. Such a statement is supported by the World Health Organization, which cited a study by The Lancet Neurology. In their report, researchers concluded that over 80% of neurological deaths occur within low and middle income countries, which indicates that the overwhelming number of people did not have access to preemptive care. Undoubtedly, this lack of neuroprotective aid can lead to dangerous outcomes because, without proper remediation and understanding, further declines in quality of life, mental health stigma, and death may occur.
Such a limited resource becomes even more alarming when we consider how fewer than 20% of the total population living in impoverished regions can afford neuropsychological assessments. In conjunction with the earlier statistic by The Lancet Neurology, such staggering data are vital to review, as they demonstrate that those who need neurological equipment the most are the ones who receive it the least. Instead, wealthy countries have more access to these evaluations as at least 80% of individuals are able to afford all neuropsychological tests. With that being said, if no policy change is implemented to bring forth more support, mental health education, and neurodiagnostic supplies to these vulnerable populations, the death toll may rise. Therefore, ensuring adequate and accessible psychological care in disenfranchised communities could mitigate this issue as it could lead to earlier prognoses, and better methods of disseminating information about neurological conditions to the public.
Ultimately, the brain and our behavior influence how we think, act, and socialize with others. Such a relationship becomes more pronounced the older we get and the more we experience stronger symptoms of cognitive decline. Consequently, having clinical neuropsychology services readily available to treat memory loss and neurodegenerative conditions, especially in regions where it is a scarcity, becomes that much more critical to integrate into society.
Sources:
- Clinical Neuropsychology
- Important of Neuropsychological Testing in Correct Diagnosis
- The Role of Neuropsychology in the Diagnosis and Treatment of Brain Injuries
- Omega-3 fatty acids and the treatment of depression: a review of scientific evidence – PMC
- Neuropsychologic Assessment for Neurodegeneration – Practical Neurology
- Population normative data for the CERAD Word List and Victoria Stroop Test in younger- and middle-aged adults: Cross-sectional analyses from the Framingham Heart Study
- What Is a Neuropsychologist? What They Do & Education
- Over 1 in 3 people affected by neurological conditions, the leading cause of illness and disability worldwide
- Availability, accessibility, and affordability of neurodiagnostic tests in 37 countries – PMC
